VOS thanks our
2018 Annual Meeting participants
VOS has adopted an Opioid Prescription Policy
Precautions:
1) Narcotics can be habit forming and addiction, tolerance or dependence can occur with longer term use
2) Combining narcotic pain medication with alcohol, sedatives, muscle relaxants, or antidepressants may result in serious side effects or complications.
3) Other medications may also have unrecognized or unpredictable interactions with pain medications.
4) Operating heavy equipment or driving is not permitted when using narcotic pain medications.
Scope of prescribing and timing of prescriptions:
1) Orthopaedic providers may prescribe pain medications for a limited time as part of treatment associated with acute injuries or surgical care/procedures.
2) As narcotics can be habit forming and addiction, tolerance or dependence can occur with longer term use, long term prescription for narcotic medications will not be provided by Orthopaedic providers beyond 90 days of use.
3) Prescriptions for narcotics/controlled substances can only be provided as a WRITTEN prescription. They may not be “called in” to a pharmacy.
4) Long term pain medication needs will require referral to pain management or the patients primary care provider.
5) Orthopaedic providers in the Commonwealth of Virginia participate in Virginia’s Prescription Monitoring Program (PMP) to allow review of physician prescribing patterns and patient narcotic use compliance.
Patient responsibilities:
1) Medications are to be used as prescribed.
2) If medications are not adequate for pain control, adjustments/increases in the amount of medication used should not be done without
discussion with the prescribing provider.
3) Failure to follow a recommended plan of treatment, including delays in advised care or surgical intervention will result in cessation of providing prescriptions for pain medication
4) Obtaining additional pain medication from another provider after prescriptions have been provided by the current orthopaedic provider is not permitted.
5) Obtaining pain medications from multiple providers (unless the “other provider” is a recognized Pain Management specialist or Primary Care provider and the current orthopaedic provider has been informed of ongoing chronic pain management) will result in the refusal to provide any additional pain medication prescriptions and contact with the other prescription provider. It may result in discharge from orthopaedic care.
6) Pain medications should be obtained from a single pharmacy.
Medication/Prescription Refills:
1) Refills of pain medications may be prescribed if appropriate.
2) Medication refills may be requested Monday-Friday during normal office hours. As it may take up to 24 hours for review of refill requests, some refills may not be completed until the next full office day.
3) Medication refills (including late requests) are not available evenings or on weekends or holidays.
4) An “On Call” provider WILL NOT refill prescriptions for pain medications.
5) Medication refills will not be provided because of missed or cancelled appointments.
6) Pain medication refills must be obtained in person by the patient, unless the patient authorizes another party to pick up the medication. This person must be listed in the chart and must bring a valid picture identification.
7) It is preferable to have patients contact a single pharmacy and have the pharmacy leave a refill message with the prescribing Orthopaedic provider Insert phone #s. Patients may leave a refill request at these numbers as well. The following information must be provided for refill messages with refill requests:
Patient Name
Patient Telephone Number
Physician name (for this prescription refill request)
Name of medication
Date of last prescription for this medication
Pharmacy name AND PHONE NUMBER
Any questions or concerns regarding these policies should be discussed in person with the Orthopaedic provider responsible for your current care during office visits.
How MSV is Combatting Opioid Misuse
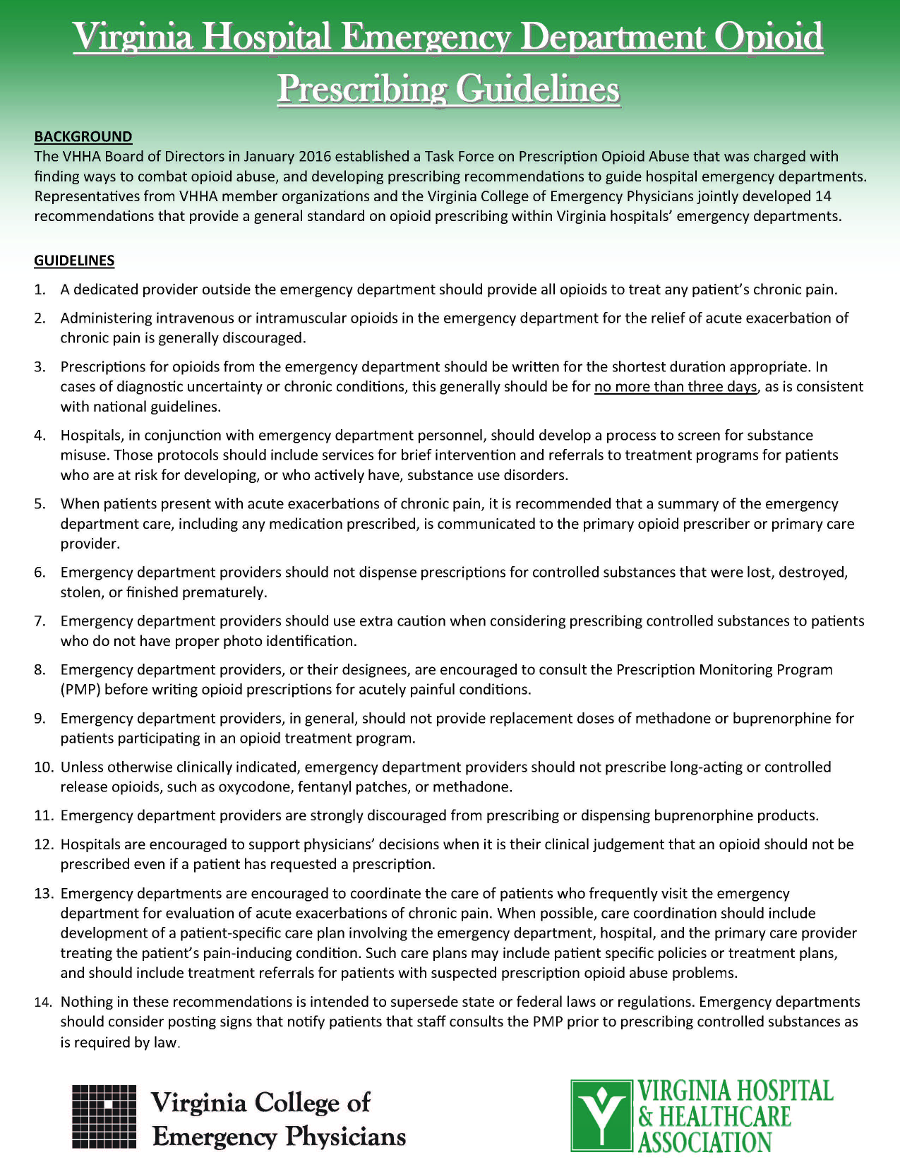
Drug overdose death rates in the United States have increased five-fold since 1980. Prescription drugs, especially opioid analgesics, have been increasingly involved in drug overdose deaths.2 Drug abuse and addiction are claiming the lives of more Virginians and have led to an increased burden on elevated health care costs from drug-related emergency department visits and treatment admissions. Opioid-related overdose deaths now outnumber overdose deaths involving all illicit drugs such as heroin and cocaine combined.
Strategies to address these issues require a multi-pronged approach and coordinated effort amongst multiple stakeholders, which is why Medical Society of Virginia (MSV) President William C. Reha, M.D., M.B.A. and the MSV Board of Directors appointed the MSV Opioid Misuse Task Force earlier this year. This group was tasked with identifying opportunities for MSV to take a leadership role in creating public awareness, developing education education and resources, and identifying prescriber and patient protections.
The governor has also identified opioid and heroin dependence as a major concern for the commonwealth. In 2014, Governor McAuliffe established the Governor’s Task Force on Prescription Drug and Heroin Abuse to recommend immediate steps to address a growing and dangerous epidemic of prescription opioid and heroin abuse in Virginia, with the ultimate goal of improving public safety and public health. The governor’s task force recently completed their work and submitted formal recommendations for his consideration. A number of legislative and public health strategies are expected to be carried forward, including a requirement that prescribers participate in continuing medical education on appropriate opioid prescribing. The full recommendations are available here.
Within the context of the state work and in consideration of the growing problem both groups are working to address, the MSV task force presented a number of recommendations to the board at its September meeting. The board adopted the recommendations, which will be available for discussion at the 2015 MSV Annual Meeting. Ideas that were presented, that will be further prioritized by the board based on available resources, include the following.
- Supporting prescriber education:
MSV should support that Virginia’s prescriber licensing bodies (the Virginia Board of Medicine, the Virginia Board of Nursing, and the Virginia Board of Dentistry) be granted the statutory authority to require specific topic-area continuing education of licensees regarding opioid prescribing and/or addiction education. The development of any such requirements should be undertaken in collaboration with public health experts and the relevant professional and specialty organizations, include provisions for measuring the effect of implementing the requirements as compared to the desired outcome, and incorporate an appropriate sunset clause. Further, the licensing bodies should be mindful of current specialty training requirements that may already address the concern, such as maintenance of board certification. In response to any such requirements, the MSV should strive to make the prescribed programming easily accessible and affordable for its members. - Assisting with patient education:
MSV will participate in efforts to educate the public regarding this epidemic, such as the promotion of patient education materials on safeguards for the treatment of chronic pain, proper use and disposal of medications and non-pharmacologic modalities for managing pain. - Enhancing prescriber education:
MSV will support a collaborative, targeted approach to prescriber education that incentivizes providers to grow their knowledgebase in this area. For instance, MSV may want to partner with medical schools, medical staffs, liability carriers, the Virginia Prescription Monitoring Program and others to offer conveniently available educational programming and feedback. - Promoting use of electronic tools to mitigate risk:
MSV believes all prescribers should voluntarily utilize the prescription monitoring program as a risk management tool, and will encourage opportunities for improving utilization. Additional opportunities include education regarding the Drug Enforcement Administration standard for electronic submission of controlled substances and encouraging electronic health record companies to provide a real-time interface with the state prescription monitoring program. - Supporting non-punitive approaches to addressing substance use disorder:
MSV recognizes that addiction is a medical condition that requires treatment. MSV will consider opportunities to improve access to and coverage for improved coverage of screening and treatment.